วันที่ created 29 พ.ย. 2568 09:31 วันที่ edited 5 ธ.ค. 2568 21:57 | เข้าชมแล้ว 372 | admin3
A 46-year-old Thai woman presents with a 6-month history of painful swelling and tightness in her hands, wrists, and elbows with morning stiffness for over 2 hours.
- She noticed her fingers turn white and numb when exposed to cold, followed by bluish-purple discoloration and then intense redness on rewarming.
- She has heartburn, early satiety, and intermittent dysphagia for solids.
- She denies oral ulcers, photosensitivity, or alopecia.

Physical examination: BT 37.0 C, RR 22/min, BP 132/84 mmHg, PR 94/min
- Diffuse edema and skin thickening and tightening extending from fingers (sclerodactyly) to proximal to the metacarpophalangeal (MCP) joints and elbows
- Cold extremities with delayed capillary refill with cyanotic discoloration of distal phalanges with digital ulcers
- Tenderness and synovitis of the MCP, PIP, and wrist joints bilaterally
- Bibasilar crackles at both lungs with questionable loud P2
- No facial rash, no photosensitivity rash, no rheumatoid nodules
- No proximal muscle weakness
Questions:
1. What is the provisional diagnosis?
2. What are the proper next step investigations?
3. What is your plan for initial treatment?
โดย น.อ.หญิง อินทิรา อุไรเลิศ อายุรแพทย์โรคข้อและรูมาติสซั่ม กองอายุรกรรม รพ.ภูมิพลอดุลยเดช กรมแพทย์ทหารอากาศ
ANSWERs
1. Provisional diagnosis: Diffuse Cutaneous Systemic Sclerosis (dcSSc)
Rationale:
1.1 Diffuse skin thickening:
- Definite criteria for diagnosis of SSc by 2013 ACR/EULAR classification criteria : skin thickening proximal to the MCP joints (score = 9, SSc classified without further scoring).
- Skin thickening extending proximal to the elbows classifies the disease as the diffuse subtype (dcSSc)
1.2 Vasculopathy: Raynaud's phenomenon, digital ulcers, delayed capillary refill
- Raynaud's phenomenon is a classic and often the earliest symptom of SSc. The description of this patient perfectly fits the triphasic color change of secondary Raynaud's.
- White and numb (Pallor/Ischemia): due to vasospasm
- Bluish-purple (Cyanosis): due to sluggish, deoxygenated blood flow
- Intense redness (Rubor): due to rapid reperfusion/rewarming
1.3 Multisystem Involvement: The patient has simultaneous involvement of the vascular system (vasculopathy), the musculoskeletal system (inflammatory arthritis/synovitis, ≥2 hours morning stiffness), the gastrointestinal tract (heartburn, dysphagia, early satiety), and the cardiopulmonary system (bibasilar crackles suggesting interstitial lung disease (ILD), loud P2 suggesting pulmonary hypertension (PH)).
1.4 The denial of oral ulcers, photosensitivity, and alopecia helps to make systemic lupus erythematosus (SLE) less likely. The absence of proximal muscle weakness makes mixed connective tissue disease (MCTD) and autoimmune myositis (AIM) less likely as the primary provisional diagnosis.
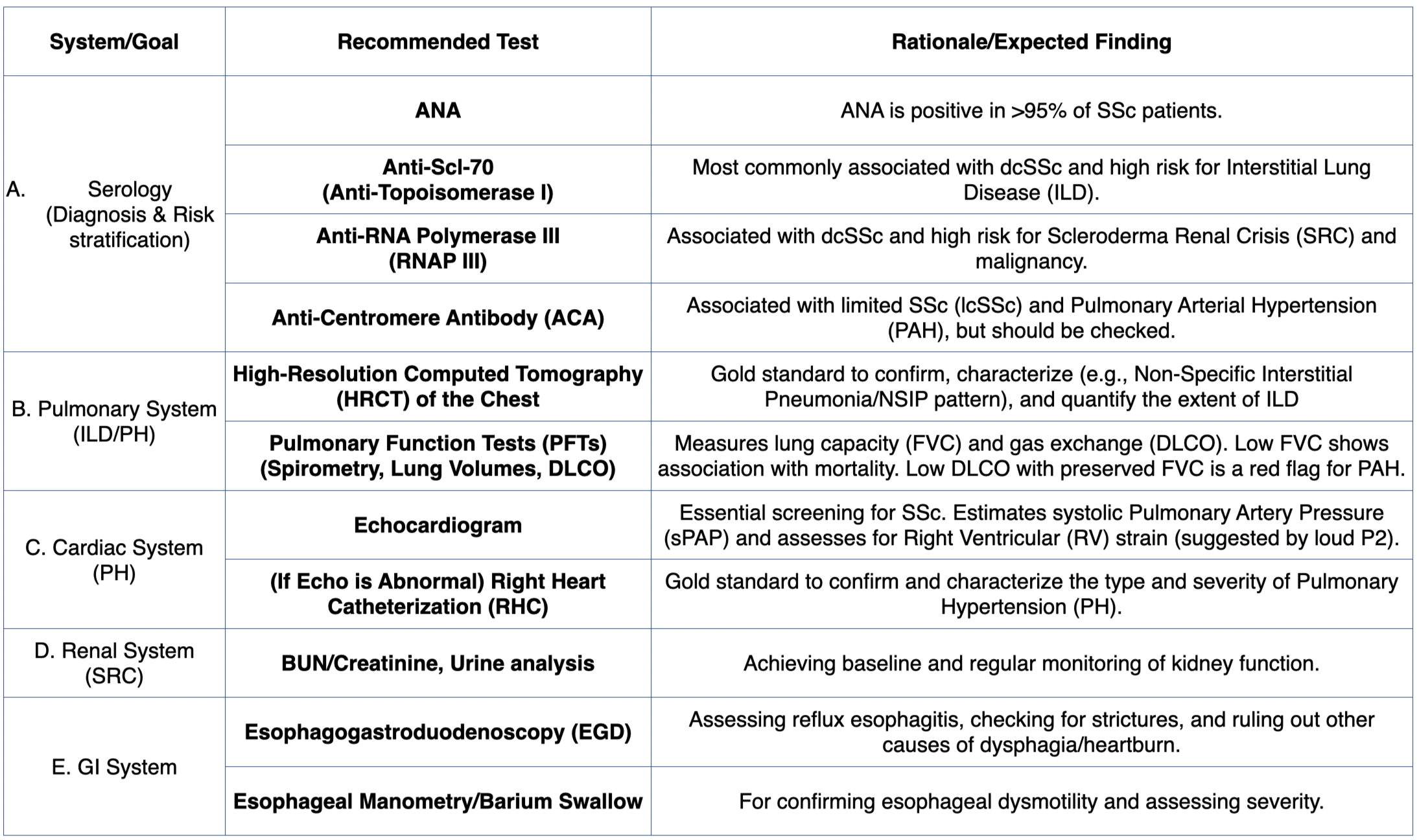
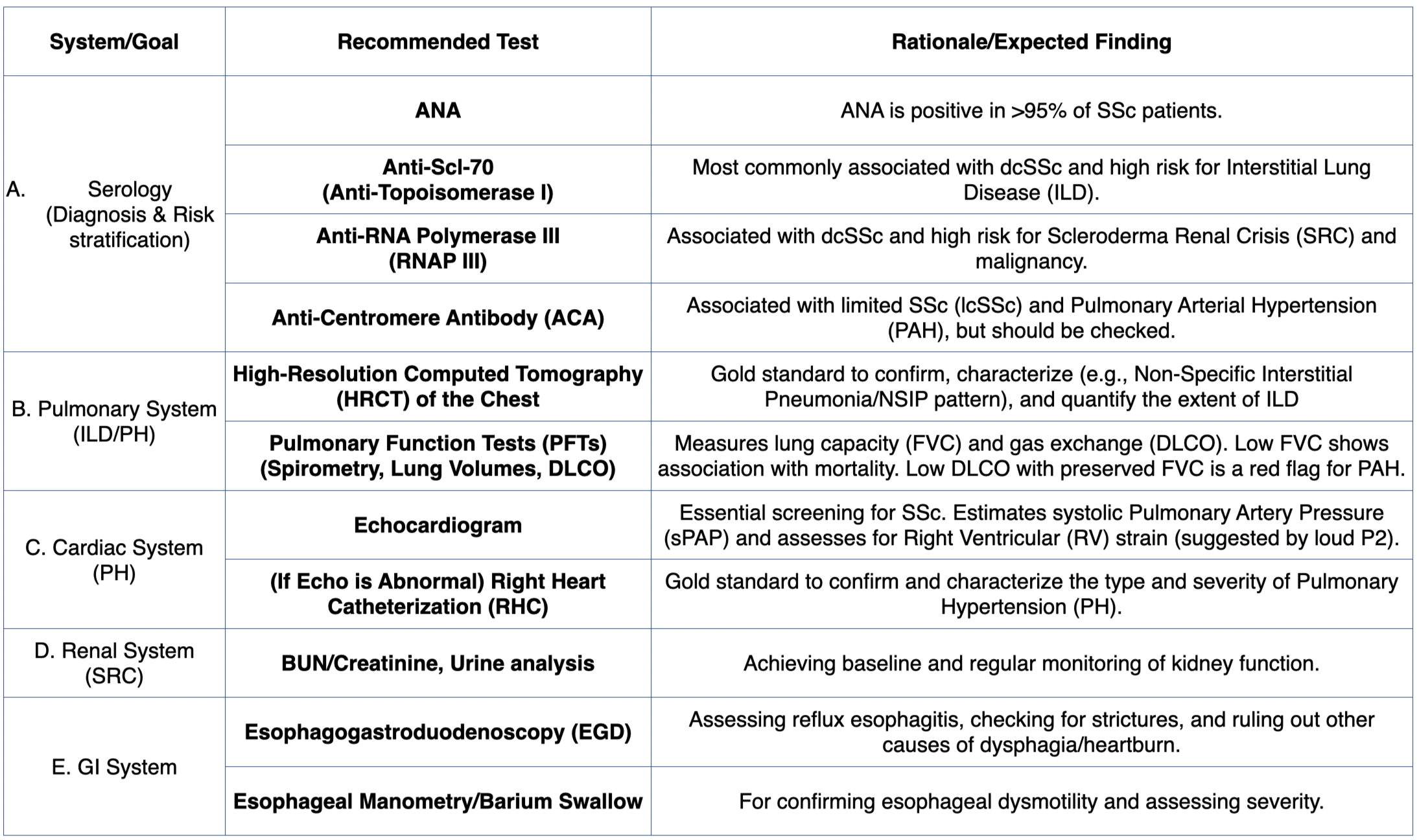
2. Next step investigations: The investigation strategy is aimed at confirming SSc and, critically, assessing the extent and severity of internal organ disease (especially lung and heart).
3. Plan for initial treatment:
3.1 Specific treatment:
- Raynaud's phenomenon : long acting dihydropyridine-type calcium channel blockers (oral nifedipine) as first line treatment; others include PDE5-inhibitors (PDE5i), topical nitrate, bosentan, and iloprost IV.
- Digital ulcers : combination therapy of above medications and start aspirin
- Refractory digital ulcers or impending digital loss : local injection of lidocaine, bupivocaine, start IV heparin drip, surgery (sympatectomy or angioplasty)
- Skin : Immunosuppresive agent (methotrexate (MTX) (1B), mycophenolate mofetil (MMF) (1B) and/or rituximab (RTX) (1A), tocilizumab (TCZ)); note that MTX can treat skin and joint disease without progression of existing ILD, however, it is rarely associated with idiosyncratic hypersensitivity pneumonitis (0.5-2%).
- Arthritis : MTX
- If confirmed ILD : Immunosuppresive agent (MMF preferred (or CY or RTX or TCZ)) with lowest possible dose of corticosteroid (none or <10 mg/day of prednisolone), may start upfront anti-fibrotic agent (nintedanib) or add later-on during monitoring.
- If confirmed PAH (PH gr. I) : Combination of PDE5i + endothelin receptor antagonist (ERA) as first-line treatment; others include prostacyclin agonist (PRA) (IV, inhaled, SC), riociguat; referral for lung transplanation in refractory functional class IV
- Gastrointestinal : PPI, H2 blockers, prokinetics
3.2 Supportive treatment:
- Raynaud's phenomenon : avoid triggers (cold, smoking, trauma, vasoconstrictors), proper clothing (gloves, stockings)
- Skin : emoilient
- SSc-ILD and PH : cardiopulmonary rehabilitation, PJP prophylaxis, vaccines (Flu, COVID19, Zoster, Pneumococcal, RSV), chest physiotherapy and airway clearance, smoking cessation, supplemental oxygen in selected cases, resistance training exercise
- GERD and motility disorder : lifestyle modification
References
- Van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, et al. 2013 classification criteria for systemic sclerosis: an ACR/EULAR collaborative initiative. Arthritis Rheum. 2013;65(11):2737-2747.
- Kachroo P, Chung L. The clinical utility of autoantibodies in systemic sclerosis: a review with a focus on cohort differences and standardization. Rheumatology. 2023;62(7):2378–2388.
- American Thoracic Society (ATS). Treatment of systemic sclerosis–associated interstitial lung disease: evidence-based recommendations. Am J Respir Crit Care Med. 2024;209(5):551–567.
- Del Galdo, F., Lescoat, A., Conaghan, P. G., et al. (2024). EULAR recommendations for the treatment of systemic sclerosis: 2023 update. Annals of the Rheumatic Diseases, 83(6), 705–719.
โดย ร.อ.หญิง ณัฐวดี มุ่งการดี แพทย์ประจำบ้านกองอายุรกรรม และ น.อ.หญิง อินทิรา อุไรเลิศ อายุรแพทย์โรคข้อและรูมาติสซั่ม กองอายุรกรรม รพ.ภูมิพลอดุลยเดช กรมแพทย์ทหารอากาศ